November Is American Diabetes Month: Know Your Numbers
About one in four adults with diabetes don’t know they have the disease. Another estimated 96 million American adults have prediabetes, which means their blood glucose levels are higher than normal but not high enough to be diagnosed as diabetes. Knowing and monitoring blood glucose levels is important. Additionally, tracking other critical health numbers can help lower your risk of diabetes complications.
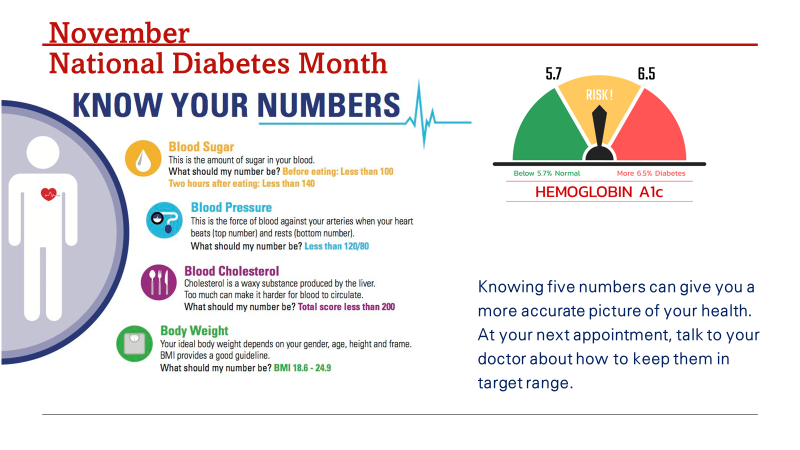
What Numbers Should You Know and Monitor?
Blood Sugar and A1C
The A1C test — also known as the hemoglobin A1C or HbA1c test — is a simple blood test that measures your average blood sugar levels over the past three months. It’s one of the most commonly used tests to diagnose prediabetes and diabetes, and it’s also the primary test to help you and your healthcare team manage your diabetes. Diabetes can cause blood sugar to rise to dangerous levels. Medications may be needed to manage your blood sugar.
Blood Pressure
High blood pressure is twice as likely to strike a person with diabetes. Left untreated, high blood pressure can lead to heart disease and stroke. A person with diabetes and high blood pressure is four times as likely to develop heart disease than someone who does not have either condition. Review this page from Johns Hopkins Medicine for information on preventing and treating high blood pressure.
Blood Cholesterol
Diabetes tends to lower “good” cholesterol levels and raise triglycerides and “bad” cholesterol levels, thereby increasing the risk of heart disease and stroke. It’s a combination that puts people at risk for premature coronary heart disease and atherosclerosis. Learning how to prevent and treat abnormal cholesterol levels is an important step in maintaining optimum health.
Body Weight/Body Mass Index (BMI)
Two measurements you can use to easily gauge if your weight is in a healthy range are body mass index (BMI) and waist circumference.
- BMI. Because calculation requires only height and weight, BMI is a very simple measurement to take. A healthy weight is defined as a BMI between 18.5 and 24.9. A weight within this BMI range is linked to fewer health problems than those in the underweight, overweight or obese ranges.
- Waist Circumference. Another way to estimate your potential disease risk is to measure your waist circumference. Having excessive abdominal fat may put you at greater risk for developing obesity-related conditions, including type 2 diabetes, high blood pressure and coronary artery disease.
How much weight do I need to lose to make a difference?
Losing weight doesn’t have to mean losing a lot of weight. Small steps can make a big difference. Shedding just 5% to 10% — that’s 10 to 20 pounds for a 200-pound person — can improve your health and wellbeing. If you have diabetes, you may find your blood sugar levels are easier to manage and that you need less diabetes medicine after you lose weight.
NOTE: Another important thing to track is physical activity. Exercising can help prevent or delay the onset of type 2 diabetes, reduce blood pressure, and even reduce the risk of heart attack and stroke. Any moderate-to-vigorous physical exercise — including playing sports, doing housework, gardening and performing work-related physical activity — is beneficial. According to the American Heart Association, the goal is to get at least 150 minutes of moderate-intensity physical activity per week. One way to do this is to try to fit in at least 20 to 25 minutes of activity daily. Also, on two or more days a week, include movements that work all major muscle groups (legs, hips, back, abdomen, chest, shoulders and arms).
Want to learn more?
- Consider reading up on the Know Diabetes by Heart™ initiative. The American Heart Association and the American Diabetes Association, along with industry leaders, are working together to reduce cardiovascular deaths, heart attacks, heart failure and strokes in people living with type 2 diabetes. The initiative seeks to comprehensively combat the national public health impact of type 2 diabetes and cardiovascular disease. Sign up for their newsletter and/or enroll in their e-learning course.
- Managing diabetes during the holidays: Use these tips to help loved ones embrace healthy food. Find suggestions to help work in fruits, veggies and more for heart-healthy meals this season. Additionally, watch this episode to help you balance festive fun with health.
As the month comes to a close, let’s do a quick recap. Below are links to other American Diabetes Month–related information and resources. We hope you found this series helpful and that you make plans to prioritize your self-care this season.
- November Is American Diabetes Month
- November Is American Diabetes Month: Eat Well
- November Is American Diabetes Month: Getting Over Hurdles to Stay Active
- CommonHealth Wellnote: Healthy Eating, Your Blood Sugar and More
Submitted by:
Dahlia Henry-Tett, Chief Wellness Officer (CWO), employeewellbeing@nvcc.edu
